Discovering unwelcome bumps on your buttocks can be a frustrating, even embarrassing, experience. Whether you’re preparing for a beach vacation, a special occasion, or simply want to feel more confident in your everyday wear, those pesky pimples can put a damper on things. But fear not! This comprehensive guide is here to illuminate the best treatment for pimples on buttocks, offering effective solutions and practical advice to reclaim your smooth, clear skin. We’ll delve into the causes, explore a range of proven remedies, and equip you with the knowledge to banish these blemishes for good.
Understanding the Culprits: Why Do Butt Pimples Appear?
Before we dive into the best treatment for pimples on buttocks, it’s crucial to understand what might be causing them. Unlike facial acne, butt pimples, often referred to as "buttne," have distinct contributing factors. While they can sometimes be true acne (caused by clogged pores and bacteria), they are frequently a form of folliculitis.
Folliculitis: The Common Culprit
Folliculitis is an inflammation of the hair follicles, the tiny sacs from which hair grows. When these follicles become infected, irritated, or blocked, they can develop into small, red bumps that resemble pimples. These can be itchy, sore, and sometimes even filled with pus.
Several factors can lead to folliculitis on the buttocks:
- Friction: Tight clothing, especially synthetic fabrics that don’t allow skin to breathe, can rub against the skin and irritate hair follicles. This is particularly common during exercise or prolonged sitting.
- Sweat: Trapped moisture from sweat can create a breeding ground for bacteria and yeast, leading to inflammation.
- Irritation from Products: Harsh soaps, laundry detergents, or fabric softeners can irritate the delicate skin on your buttocks, triggering folliculitis.
- Ingrown Hairs: Shaving, waxing, or even tight clothing can cause hairs to curl back and grow into the skin, leading to inflamed bumps.
- Bacteria and Yeast: Staphylococcus aureus (Staph) is a common bacterium that can infect hair follicles. Certain types of yeast can also contribute to folliculitis.
- Blocked Pores: Similar to facial acne, dead skin cells, oil (sebum), and dirt can clog pores and hair follicles, leading to breakouts.
True Acne vs. Folliculitis: A Subtle Distinction
While the visual appearance can be similar, true acne typically involves the sebaceous glands, which produce oil. Folliculitis, on the other hand, is primarily an issue with the hair follicle itself. Identifying the difference can sometimes help in choosing the most effective treatment. If your bumps are more widespread, itchy, and don’t have a distinct "head" like a traditional pimple, folliculitis is a strong possibility.
The Quest for Clear Skin: Best Treatment for Pimples on Buttocks Unveiled
Now that we understand the potential causes, let’s explore the most effective strategies for tackling those stubborn butt pimples. The best treatment for pimples on buttocks often involves a multi-pronged approach, combining topical remedies, lifestyle adjustments, and sometimes, medical intervention.
1. Gentle Cleansing: The Foundation of Clear Skin
The first and most crucial step in any treatment plan is proper hygiene.
Daily Washing with a Gentle Cleanser
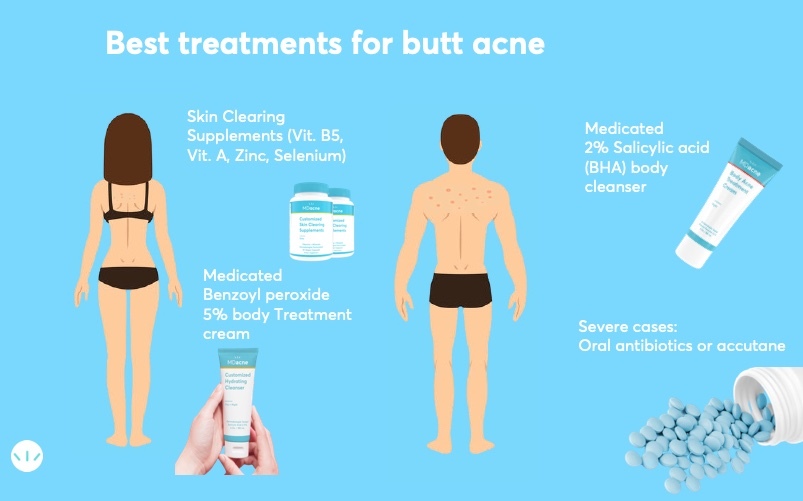
- What to look for: Opt for a mild, fragrance-free body wash or soap. Avoid harsh, stripping cleansers that can exacerbate irritation. Look for ingredients like salicylic acid or benzoyl peroxide, which are excellent for combating acne and folliculitis.
- How to use it: Wash your buttocks daily, especially after sweating. Use lukewarm water and your hands or a soft washcloth. Gently lather and rinse thoroughly. Pat your skin dry with a clean towel – avoid vigorous rubbing.
Exfoliation: Removing Dead Skin Cells
- Chemical Exfoliants: These are often more effective and less irritating than physical scrubs for butt acne.
- Salicylic Acid (BHA): This oil-soluble ingredient can penetrate pores and hair follicles to unclog them. It also has anti-inflammatory properties. Look for body washes, lotions, or pads containing 1-2% salicylic acid.
- Glycolic Acid (AHA): This alpha-hydroxy acid helps to slough off dead skin cells from the surface, revealing smoother skin and preventing future blockages. Glycolic acid toners or lotions can be beneficial.
- Physical Exfoliants (Use with Caution): If you choose to use a scrub, opt for one with fine, smooth particles (like sugar or finely ground oats) and use it very gently, no more than 1-2 times per week. Avoid harsh scrubs with large, jagged particles that can cause micro-tears and worsen inflammation.
2. Topical Treatments: Targeting the Blemishes
Once your skin is clean, applying targeted treatments can accelerate healing and prevent new breakouts.
Over-the-Counter (OTC) Medications
- Benzoyl Peroxide: This powerful ingredient kills acne-causing bacteria and helps to unclog pores. It’s available in various strengths (2.5% to 10%). Start with a lower concentration to minimize dryness and irritation. Apply a thin layer to affected areas after cleansing. Be aware that benzoyl peroxide can bleach fabrics, so wear old pajamas or use a white towel.
- Topical Antibiotics: For bacterial folliculitis, OTC antibiotic creams or ointments containing ingredients like bacitracin or neomycin can be helpful. However, their effectiveness can be limited for deeper infections.
- Hydrocortisone Cream: For very itchy or inflamed bumps, a low-strength hydrocortisone cream (0.5% or 1%) can provide temporary relief. Use it sparingly and for short periods, as prolonged use can thin the skin.
Prescription Topical Treatments
If OTC options aren’t sufficient, a dermatologist may prescribe stronger treatments:
- Topical Antibiotics (Prescription Strength): Clindamycin or erythromycin are commonly prescribed to kill bacteria.
- Topical Retinoids: These vitamin A derivatives (like tretinoin or adapalene) help to unclog pores, reduce inflammation, and promote cell turnover. They can be very effective but may cause initial dryness and peeling.
- Antifungal Creams: If yeast is suspected as the cause of folliculitis, antifungal creams like clotrimazole or ketoconazole may be prescribed.
3. Lifestyle Modifications: Prevention is Key
The best treatment for pimples on buttocks isn’t just about what you apply; it’s also about how you live. Making conscious changes can significantly reduce the frequency and severity of breakouts.
Clothing Choices Matter
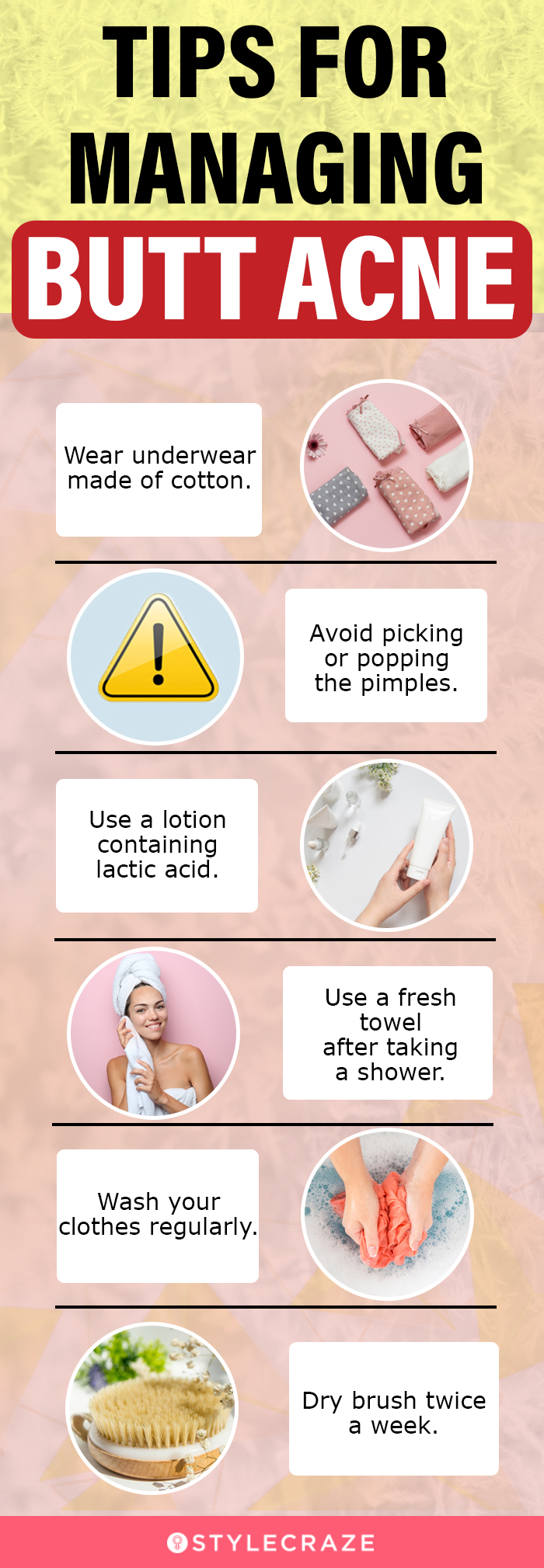
- Breathable Fabrics: Prioritize cotton, linen, or moisture-wicking synthetic fabrics for your underwear and loungewear. These materials allow air to circulate and help to keep the area dry.
- Avoid Tight Clothing: Looser-fitting pants, shorts, and skirts can reduce friction and irritation. If you wear tight workout gear, change into something looser and breathable as soon as possible after your exercise session.
- Clean Underwear Daily: Always wear clean underwear, and change it daily or more often if it becomes damp.
Hygiene Habits
- Shower After Sweating: Don’t let sweat linger on your skin. Shower immediately after workouts or any activity that causes you to sweat heavily.
- Gentle Drying: After showering, pat your skin dry with a clean towel. Avoid rubbing, which can irritate the skin and spread bacteria.
- Wash Workout Clothes Promptly: Don’t let sweaty gym clothes sit in your hamper. Wash them as soon as possible to prevent bacterial growth.
Sitting Habits
- Avoid Prolonged Sitting: If your job requires long periods of sitting, try to get up and move around regularly. This allows for better air circulation and reduces pressure on the area.
- Consider a Breathable Seat Cushion: If prolonged sitting is unavoidable, a breathable cushion might offer some relief.
Shaving and Hair Removal
- Consider Alternatives: If shaving or waxing is a trigger, explore other hair removal methods like trimming or epilating, or consider laser hair removal for a more permanent solution.
- Proper Technique: If you must shave, use a sharp, clean razor, shave in the direction of hair growth, and always use a shaving cream or gel to lubricate the skin. Exfoliate gently before shaving to help prevent ingrown hairs.
4. Home Remedies and Natural Approaches
While not always a substitute for medical How to get rid of razor bumps fast women unlock silky smooth skin now treatment, some natural remedies can complement your routine.
Warm Compresses
- How it helps: Applying a warm compress can help to draw out infection, reduce inflammation, and soothe discomfort.
- How to use it: Soak a clean washcloth in warm water, wring it out, and apply it to the affected area for 10-15 minutes, several times a day.
Tea Tree Oil
- Properties: Tea tree oil has natural antibacterial and anti-inflammatory properties.
- How to use it: Always dilute tea tree oil with a carrier oil (like coconut or jojoba oil) before applying it to the skin. A common dilution is 1-2 drops of tea tree oil per teaspoon of carrier oil. Apply with a cotton swab to individual pimples. Perform a patch test first to ensure you don’t have a reaction.
Apple Cider Vinegar (Diluted)
- Properties: Apple cider vinegar has antiseptic properties.
- How to use it: Dilute apple cider vinegar with water (start with a 1:3 ratio of ACV to water). Apply to the affected area with a cotton ball. Leave it on for a few minutes before rinsing. Use with caution, as it can be drying and irritating if not properly diluted.
5. When to Seek Professional Help
While many butt pimples can be managed at home, it’s important to know when to consult a healthcare professional.
Persistent or Worsening Breakouts
If your pimples don’t improve after several weeks of home treatment, or if they become more numerous, painful, or inflamed, it’s time to see a doctor or dermatologist.
Signs of Infection
Seek medical attention if you notice any signs of a more serious infection, such as:
- Increasing redness and swelling
- Warmth around the affected area
- Fever or chills
- Pus that is thick and yellow or green
- Severe pain
Recurrent Issues
If you experience frequent bouts of butt pimples, a dermatologist can help identify underlying causes and develop a long-term management plan. They may prescribe oral medications like antibiotics or isotretinoin for severe or persistent cases.
Embracing Confidence: Living with Clearer Skin
Dealing with pimples on your buttocks can be a confidence-eroding issue, but remember that you’re not alone. By understanding the causes and implementing the best treatment for pimples on buttocks, you can achieve smoother, clearer skin. Be patient with the process, as it can take time to see significant results. Consistency in your skincare routine and lifestyle adjustments is key.
Don’t let these blemishes hold you back from enjoying life to the fullest. Whether it’s slipping into your favorite swimsuit or feeling comfortable in your everyday clothes, clear skin can contribute to a greater sense of well-being.
Frequently Asked Questions (FAQ)
Q1: Are butt pimples contagious?
Generally, no. While bacterial folliculitis can spread to other areas of your body if hygiene is poor, butt pimples themselves are not typically contagious in the way a viral infection is.
Q2: Can I pop butt pimples?
It’s generally not recommended to pop pimples on your buttocks. Doing so can push bacteria deeper into the follicle, leading to more inflammation, infection, and potentially scarring.
Q3: How long does it take for butt pimples to go away?
With consistent treatment, mild cases can improve within a few days to a couple of weeks. More persistent or severe cases may take longer, and prescription treatments might be necessary.
Q4: Is it normal to have pimples on your buttocks?
Yes, it’s quite common! Many people experience pimples or folliculitis on their buttocks due to factors like friction, sweat, and clothing.
Q5: What is the best way to prevent butt pimples?
The best prevention involves maintaining good hygiene, wearing breathable clothing, showering after sweating, and avoiding tight garments that cause friction. Gentle exfoliation can also help.
Q6: Can stress cause pimples on my buttocks?
While stress is more commonly linked to facial acne, it can exacerbate inflammation throughout the body, potentially contributing to breakouts in other areas, including the buttocks.
Q7: Should I see a doctor if I have butt pimples?
If your pimples are persistent, painful, worsening, or show signs of infection, it’s always a good idea to consult a doctor or dermatologist for a proper diagnosis and treatment plan.
We hope this comprehensive guide has provided you with the clarity and solutions you need to tackle butt pimples effectively. Share your experiences or any other tips you’ve found helpful in the comments below – let’s help each other achieve our clearest, most confident skin!