Ah, the dreaded under-the-skin pimple. It’s that frustrating, often painful bump that lurks beneath the surface, refusing to cooperate with your usual skincare routine. Unlike its more superficial cousins, these deep-seated blemishes can feel like an unwelcome guest that’s here to stay. But fear not! Understanding how to get under the skin pimples to reveal their secrets and finally banish them is entirely possible. This comprehensive guide will delve into the causes, effective treatments, and preventative measures to help you achieve clearer, smoother skin.
The Frustrating Reality of Subcutaneous Spots
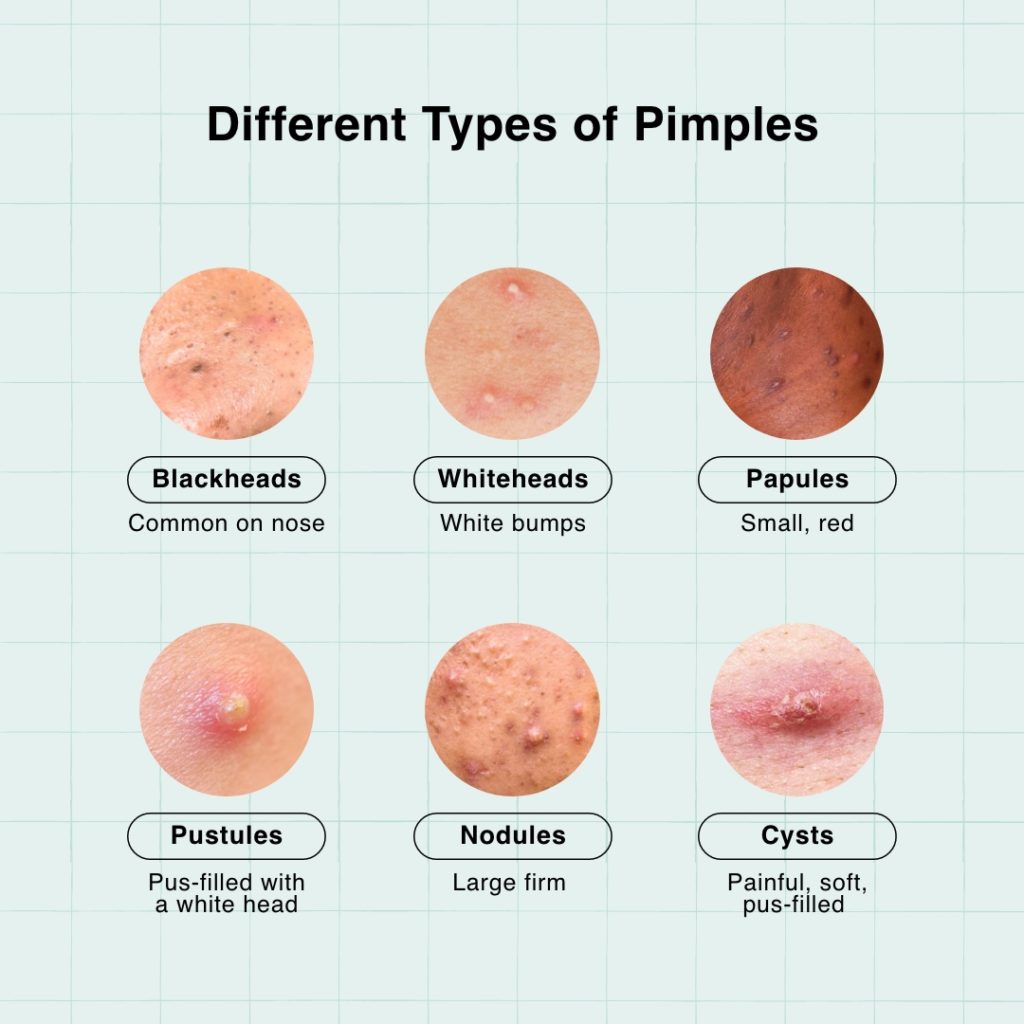
We’ve all been there. You wake up, glance in the mirror, and there it is – a tender, swollen lump that’s not quite ready to erupt. These are often referred to as cystic acne or nodules, and they represent a more severe form of acne where inflammation runs deep within the skin’s pores. Unlike whiteheads or blackheads, which have a visible opening, these subterranean invaders are trapped, leading to prolonged discomfort and potential scarring.
Unmasking the Culprits: What Causes Under the Skin Pimples?
To effectively tackle these stubborn spots, we need to understand what’s brewing beneath the surface. Several factors contribute to the formation of under-the-skin pimples:
1. The Oily Culprit: Excess Sebum Production
Our skin naturally produces an oil called sebum, which helps to keep it moisturized and protected. However, when sebaceous glands go into overdrive, they can produce too much sebum. This excess oil, combined with dead skin cells, can clog pores. When this blockage occurs deep within the hair follicle, it creates an ideal environment for bacteria to thrive, leading to inflammation and the formation of those deep, painful bumps.
2. The Dead Skin Cell Dilemma
Our skin is constantly shedding dead cells. Normally, these cells slough off unnoticed. However, if the shedding process is impaired, dead skin cells can accumulate within the pores, mixing with sebum and creating a plug. This is a common precursor to all types of acne, including those that form deep under the skin.
3. The Bacterial Invaders: Propionibacterium acnes
A type of bacteria naturally found on our skin, Propionibacterium acnes (P. acnes), plays a significant role in acne development. When pores become clogged with sebum and dead skin cells, P. acnes can multiply rapidly. This proliferation triggers an inflammatory response from the body, leading to the redness, swelling, and pain associated with under-the-skin pimples.
4. Hormonal Havoc: The Fluctuating Tide
Hormones, particularly androgens, play a crucial role in sebum production. Fluctuations in hormone levels, common during puberty, menstruation, pregnancy, and menopause, can lead to increased sebum production and, consequently, a higher likelihood of developing acne. This is why many individuals experience breakouts around their jawline and chin during their menstrual cycle.
5. The Genetics Factor: A Predisposition
If acne runs in your family, you might be genetically predisposed to developing it, including those deep, persistent pimples. While you can’t change your genes, understanding this predisposition can help you be more proactive with your skincare.
6. Stress and Lifestyle: The Unseen Triggers
While not a direct cause, stress can exacerbate existing acne conditions. When you’re stressed, your body releases cortisol, a hormone that can increase sebum production. Poor diet, lack of sleep, and certain medications can also contribute to or worsen acne.
Mastering the Art of How to Get Under the Skin Pimples to Heal
Now that we understand the "why," let’s focus on the "how." Tackling under-the-skin pimples requires a multi-pronged approach, focusing on reducing inflammation, unclogging pores, and preventing future breakouts.
H3: Gentle Yet Effective Topical Treatments
When dealing with deep-seated acne, harsh scrubbing is counterproductive. Instead, opt for targeted treatments that can penetrate the skin and address the inflammation.
Salicylic Acid: The Pore-Penetrating Powerhouse
Salicylic acid is a beta-hydroxy acid (BHA) that is oil-soluble, meaning it can effectively penetrate into the pores and break down the mixture of sebum and dead skin cells that cause blockages. It also has anti-inflammatory properties, which can help reduce the redness and swelling associated with under-the-skin pimples. Look for cleansers, toners, or spot treatments containing 1-2% salicylic acid.
Benzoyl Peroxide: The Bacterial Buster
Benzoyl peroxide is a potent ingredient that works by killing acne-causing bacteria and helping to unclog pores. It also has a mild exfoliating effect. It’s available in various concentrations, typically 2.5% to 10%. Start with a lower concentration to minimize potential dryness and irritation. Benzoyl peroxide can be effective as a spot treatment or as part of a daily cleansing routine. Be aware that it can bleach fabrics, so use it with caution around clothing and bedding.
Retinoids: The Cell Turnover Accelerators
Retinoids, derived from vitamin A, are incredibly effective at treating acne. They work by increasing cell turnover, preventing dead skin cells from clogging pores, and reducing inflammation. Over-the-counter options include retinol and adapalene. Prescription-strength retinoids like tretinoin are also available and can be highly effective for stubborn acne. Start slowly with retinoids, as they can cause initial dryness and peeling. Apply them at night, as they can make your skin more sensitive to sunlight.
H3: The Power of Professional Intervention
For persistent or severe under-the-skin pimples, consulting a dermatologist is highly recommended. They can offer advanced treatments and personalized advice.
Cortisone Injections: The Speedy Solution
For a large, painful, and inflamed under-the-skin pimple that needs to disappear quickly, a dermatologist can administer a cortisone injection directly into the lesion. This powerful anti-inflammatory medication can significantly reduce swelling and redness within 24-48 hours, offering much-needed relief.
Oral Medications: Addressing the Root Cause
In more severe cases, a dermatologist may prescribe oral medications to address the underlying causes of acne.
- Antibiotics: Oral antibiotics can help reduce the bacteria P. acnes and control inflammation. They are typically prescribed for a limited duration to prevent antibiotic resistance.
- Hormonal Therapy: For women whose acne is linked to hormonal fluctuations, oral contraceptives or anti-androgen medications can be very effective in regulating hormone levels and reducing sebum production.
- Isotretinoin (Accutane): This is a powerful oral retinoid reserved for severe, persistent, or scarring acne that hasn’t responded to other treatments. It works by significantly reducing sebum production, preventing pore clogging, and decreasing inflammation. Isotretinoin requires close medical supervision due to potential side effects.
H3: Home Remedies and Supportive Care
While professional treatments are often necessary, certain home remedies and lifestyle adjustments can complement your skincare routine and aid in the healing process.
The Soothing Power of Warm Compresses
Applying a warm, damp cloth to the affected area for 10-15 minutes, several times a day, can help bring the under-the-skin pimple to a head. The warmth can encourage the pus to rise to the surface, making it easier for the pimple to drain naturally.
The Anti-Inflammatory Magic of Tea Tree Oil
Diluted tea tree oil has natural antibacterial and anti-inflammatory properties. Mix a few drops of tea tree oil with a carrier oil like jojoba or coconut oil (a 1:9 ratio is a good starting point) and apply it to the pimple with a cotton swab. Perform a patch test first to ensure you don’t have a reaction.
The Calming Embrace of Aloe Vera
Pure aloe vera gel can help soothe inflammation and promote healing. Apply a thin layer of fresh aloe vera gel directly to the pimple.
The Importance of a Balanced Diet
While diet isn’t the sole cause of acne, some studies suggest that a diet high in refined carbohydrates and dairy may exacerbate breakouts for some individuals. Focusing on a diet rich in fruits, vegetables, and whole grains can support overall skin health.
Hydration is Key: Drink Up!
Staying well-hydrated is crucial for healthy skin. Water helps to flush out toxins and keep your skin cells functioning optimally. Aim for at least 8 glasses of water a day.
Stress Management Techniques
Incorporating stress-reducing activities like yoga, meditation, deep breathing exercises, or spending time in nature can have a positive impact on your skin by helping to regulate cortisol levels.
H3: What NOT to Do: Avoiding Pitfalls
When it comes to under-the-skin pimples, certain actions can make things worse.
The Temptation to Pop: Resist the Urge!
This is perhaps the most crucial piece of advice. Popping or squeezing an under-the-skin pimple can push the inflammation deeper into the skin, leading to increased redness, swelling, a higher risk of infection, and, most importantly, scarring. Be patient and let your chosen treatments work.
Over-Exfoliation: The Damaging Dance
While exfoliation is important, overdoing it can strip your skin of its natural oils, leading to irritation and potentially more breakouts. Stick to gentle exfoliation methods and avoid harsh scrubs.
Using Harsh Skincare Products
Avoid products with alcohol, strong fragrances, or sulfates, which can irritate and dry out your skin, potentially worsening inflammation.
Prevention is the Ultimate Strategy
Once you’ve successfully treated those stubborn under-the-skin pimples, the goal is to prevent them from returning.
H3: Establishing a Consistent Skincare Routine
A consistent and gentle skincare routine is your best defense.
Cleansing Twice Daily
Wash your face twice a day with a mild, non-comedogenic cleanser to remove excess oil, dirt, and makeup.
Moisturizing is Non-Negotiable
Even oily skin needs moisture. Use a lightweight, oil-free, and non-comedogenic moisturizer to keep your skin hydrated and prevent it from overcompensating by producing more oil.
Regular Exfoliation (Gentle!)
Incorporate a gentle chemical exfoliant (like salicylic acid or a mild AHA) into your routine 1-3 times a week to keep pores clear.
Sun Protection is Paramount
Sun exposure can worsen inflammation and hyperpigmentation, making acne scars more noticeable. Always wear a broad-spectrum SPF 30 or higher.
H3: Lifestyle Choices for Clearer Skin
Beyond your skincare routine, certain lifestyle habits can significantly impact your skin’s health.
Cleanliness is Next to Godliness (for Your Skin)
Change your pillowcases regularly (at least once a week) as they can harbor bacteria and oil. Clean your phone screen frequently, as it comes into contact with your face.
Mindful Makeup Choices
Opt for non-comedogenic makeup products that won’t clog your pores. Always remove Severe breakout on face your ultimate guide to reclaiming clear skin your makeup thoroughly before going to bed.
Healthy Habits for Healthy Skin
Prioritize sleep, manage stress, and maintain a balanced diet. These foundational elements contribute significantly to your overall well-being, including the health of your skin.
Frequently Asked Questions About Under the Skin Pimples
Q1: How long does it take for an under-the-skin pimple to go away?
A: Under-the-skin pimples, especially nodules and cysts, can take anywhere from a few days to several weeks to fully resolve. Patience and consistent treatment are key.
Q2: Can I use a pimple patch on an under-the-skin pimple?
A: Traditional pimple patches are designed for pimples with a visible head. Hydrocolloid patches can help absorb fluid from open wounds, but they are generally not effective for deep, closed under-the-skin pimples. Some specialized patches contain ingredients like salicylic acid or microneedles that might offer some benefit, but they are not a guaranteed solution for deep cysts.
Q3: Will an under-the-skin pimple leave a scar?
A: There is a risk of scarring with under-the-skin pimples, especially if they are picked at or become severely inflamed. Prompt and appropriate treatment can help minimize this risk.
Q4: Are there any quick fixes for under-the-skin pimples?
A: While cortisone injections are a fast-acting professional treatment for a single, large pimple, there are no true "quick fixes" for under-the-skin pimples at home. Relying on effective treatments and allowing your skin to heal naturally is the best approach.
Q5: When should I see a dermatologist for under-the-skin pimples?
A: You should see a dermatologist if your under-the-skin pimples are:
- Painful and inflamed
- Persistent and not responding to over-the-counter treatments
- Leading to scarring
- Affecting your self-esteem
Embrace Your Journey to Clearer Skin!
Understanding how to get under the skin pimples to heal is about patience, consistency, and the right approach. By identifying the underlying causes and employing effective treatments, you can conquer these stubborn blemishes and reveal the radiant, healthy skin you deserve. Don’t be discouraged by setbacks; celebrate your progress and embrace the journey towards a clearer complexion.
What are your biggest challenges with under-the-skin pimples? Share your experiences and tips in the comments below! Let’s help each other shine!